Benign Prostatic Hyperplasia (BPH) / Enlarged Prostate
The enlarged prostate is not caused by cancer.
An enlarged prostate is very common in men over the age of 40 years old, with roughly half having symptoms.
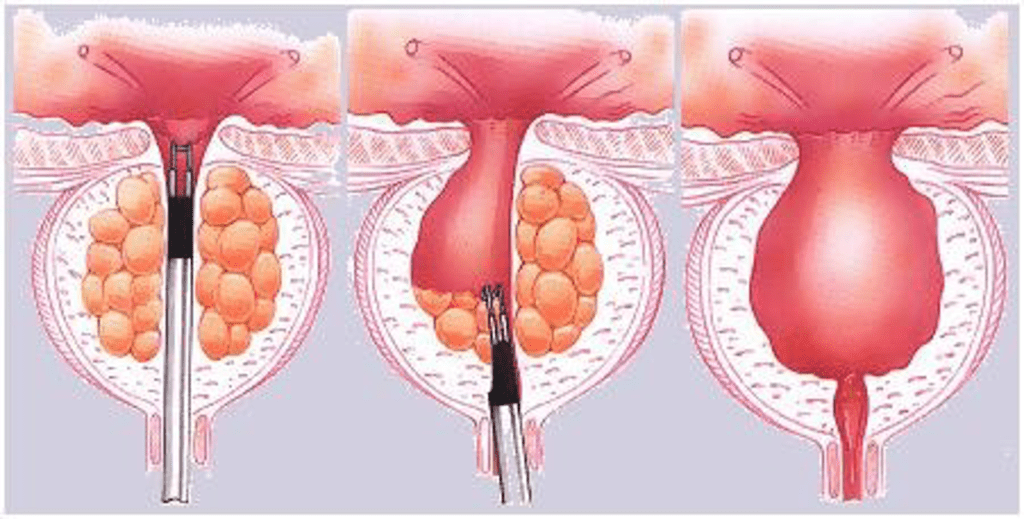
The high bladder pressures and mechanical tension seen with BPH activates chemical pathways in the bladder to compensate for the obstruction. Whilst initially COMPENSATORY, left unchecked these become DECOMPENSATORY, with remodelling of the upper and lower urinary tract, fibrous changes in the bladder muscle, and functional impairment.
What is BPH?
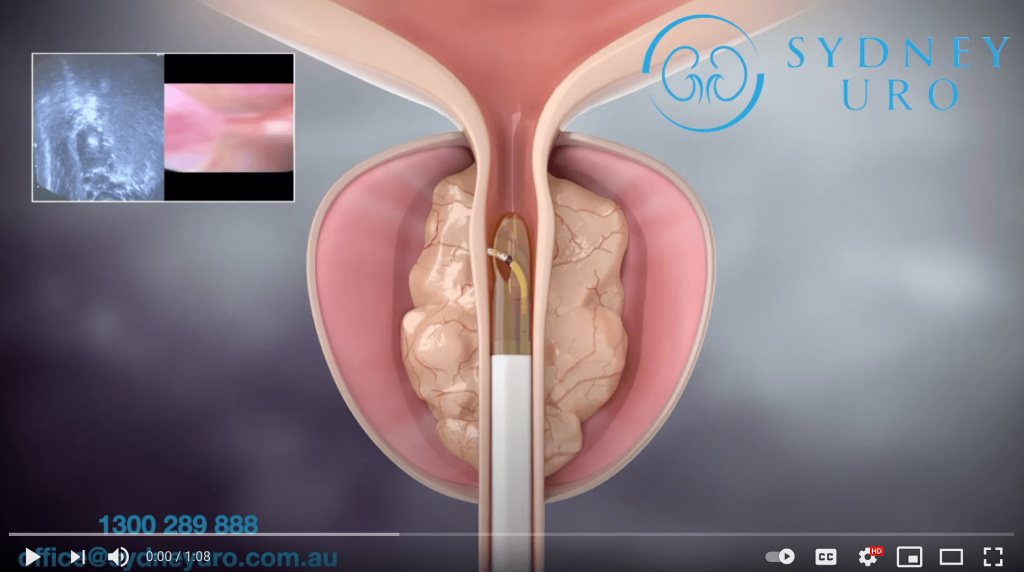
Benign Prostate Hypertrophy (BPH), and the resulting Bladder Outlet Obstruction (BOO), is considered to be the genesis of many of the problematic male Lower Urinary Tract Symptoms (LUTS).
Benign Prostate Hyperplasia (BPH) | Histological diagnosis – an increase in cell numbers when viewed under a microscope |
Benign Prostate Enlargement (BPE) | Clinical diagnosis based on DRE (finger exam) |
Bladder Outlet Obstruction (BOO) | Clinical diagnosis of altered bladder function |
Lower Urinary Tract Symptoms (LUTS) | Constellation of symptoms which is neither gender nor organ specific |
Common symptoms include:
- Weak stream
- Hesitancy to urinate
- Increased urinary urgency
- Increased urinary frequency
- Incomplete bladder emptying
- Nocturia (waking at night to urinate)
Allowed to progress further, a man might then develop more severe symptoms:
- Urinary tract infections
- Urinary incontinence (leakage of urine)
- Inability to urinate (catheter dependence)
- Haematuria (blood in the urine)
- Urinary tract infections
- Bladder stones (crystalisation of stagnant urine until multi-centimetre stones form)
- Bladder diverticulae (hernias in the bladder form)
- Renal failure / need for dialysis
The diagnosis of BPH is based on a detailed urinary tract history, a physical examination by Dr Symons or your GP, and with the aid of the International Prostate Symptom Score – please complete this and bring it with you to your appointment)
Common tests that might assist in your management include urine tests, blood tests including the PSA, and imaging (such as an ultrasound or CT).
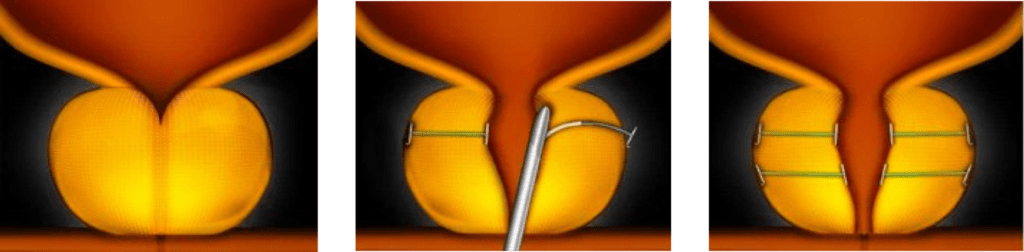
Benign Prostatic Hyperplasia (BPH) Treatments
Results from published studies indicate that both medical treatment and endoscopic surgical treatments will improve the urinary symptoms in men suffering from BPH/LUTS. However, the magnitude of improvement differs between the various treatment options – surgical procedures provide the greatest improvement in symptoms due to a greater reduction in the bladder outlet obstruction. Surgical treatments also have a much greater likelihood of reducing the progression to the more severe symptoms. From a pre-emptive health point of view, reduction of bladder outlet obstructions decreases detrusor (bladder) pressures, and helps preserve the long term integrity of the bladder itself.
There are several treatments and procedures that can be undertaken to treat BPH, please see the details of each of these below. Following a detailed personalised consultation, Dr Symons will discuss which treatment option would be most appropriate for you.